Understanding Chronic Pain: A Neurosurgical Perspective on Why Pain Persists—and What It Means for Care
By Peter A. Zahos, MD, FAANS, FACS
Board-Certified Neurosurgeon, Level One Neurosurgery
Pain Is Real—Even When Imaging Is Normal
One of the most common and distressing experiences for patients with chronic pain is being told:
“Your MRI looks normal.”
From a neurosurgical standpoint, this statement—while factually accurate—often fails to explain the patient’s lived reality. Modern neuroscience has made it clear that pain does not require visible tissue damage to be real, severe, or disabling.
What Is Chronic Pain?
In 2020, the International Association for the Study of Pain formally updated its definition of pain to reflect this understanding. Pain is now defined as:
“An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”
This definition matters. It recognizes that pain is generated and interpreted by the nervous system, not solely by injured structures. Chronic pain, therefore, is not simply a lingering symptom—it is often a condition of the nervous system itself.
Medically, chronic pain is defined as pain lasting longer than three months or beyond the normal period of tissue healing. However, duration alone does not explain chronic pain.
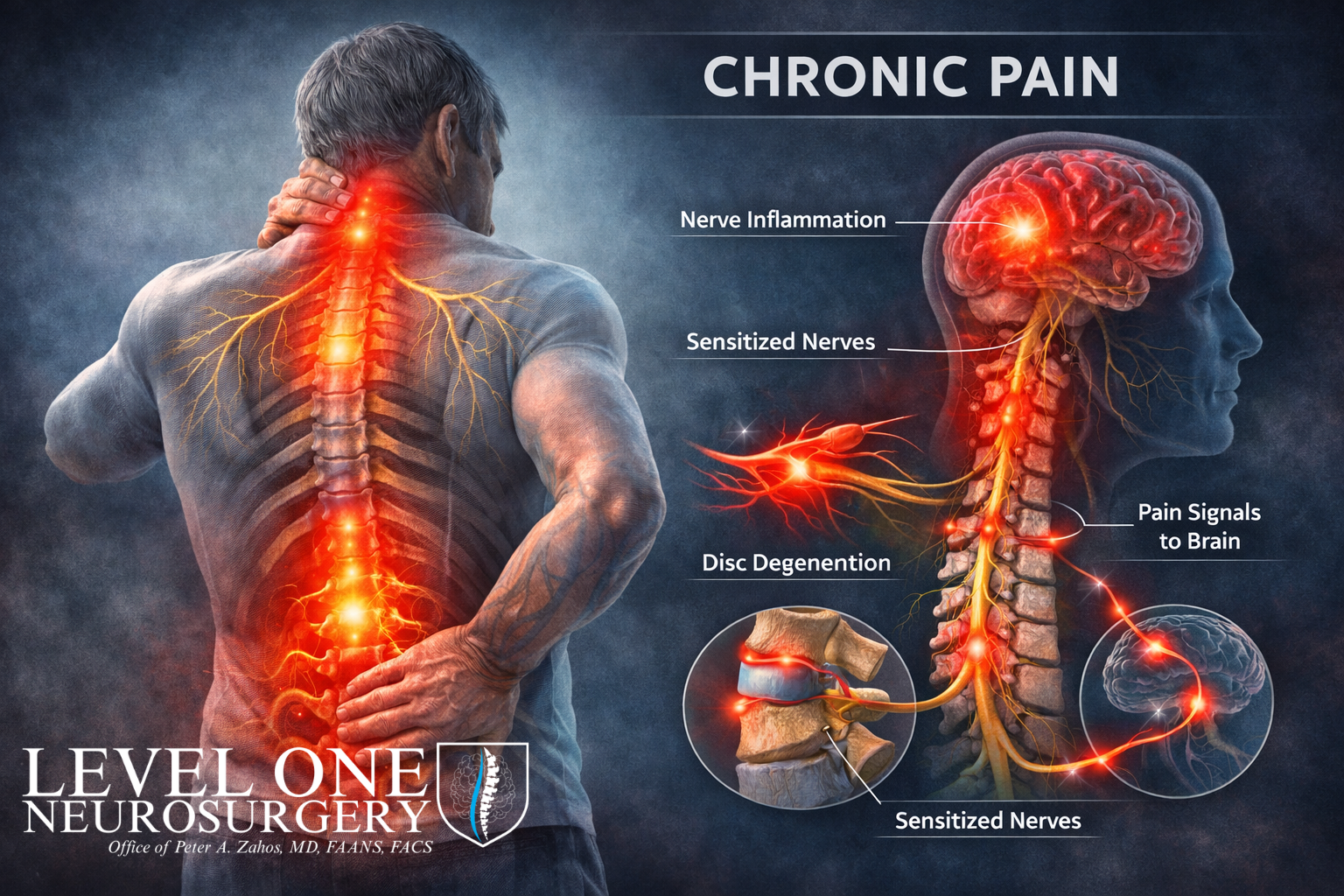
Research over the last several years has shown that chronic pain is often associated with measurable changes in the nervous system, including altered pain signaling pathways, persistent inflammation, and heightened sensitivity of nerve circuits—a process known as central sensitization (Lancet Neurology, 2021).
This means chronic pain is not imagined, exaggerated, or “all in someone’s head.” It is a real condition with identifiable biological drivers.
Common Spine-Related Causes of Chronic Pain
From a neurosurgical perspective, chronic pain frequently originates from structural or neurologic conditions, particularly within the spine..
Degenerative Disc Disease
As spinal discs degenerate, they can develop tears, lose height, or trigger inflammatory responses that stimulate nearby pain fibers. These changes can produce chronic back pain or neck pain even without a dramatic injury (BMJ, 2023).
Spinal Stenosis
Spinal stenosis occurs when the spinal canal or nerve openings narrow, compressing the spinal cord or nerve roots. This compression can lead to persistent pain, numbness, weakness, or difficulty walking, especially when untreated over time (NEJM, 2022).
Chronic Nerve Compression (Radiculopathy)
Ongoing nerve root compression may cause chronic nerve pain that persists even after the original injury has healed. Prolonged compression increases the risk of permanent nerve damage if not addressed (Spine Journal, 2023).
Spinal Instability
Abnormal motion between vertebrae can create mechanical pain and progressive neurologic symptoms, particularly during everyday activities such as standing, walking, or bending.
In many patients, imaging studies clearly demonstrate these conditions, yet they are often dismissed as “normal aging” despite a strong correlation with symptoms.
Why Chronic Pain Is Often Mismanaged
Chronic pain is frequently treated with a one-size-fits-all approach—cycling through medications, injections, or generalized therapy without reassessing the underlying cause.
Large clinical reviews now show that mechanism-based treatment, which targets the specific structural or neurologic source of pain, produces better long-term outcomes than symptom-based treatment alone (Lancet Neurology, 2021; BMJ, 2023).
Avoiding intervention simply because pain is chronic is not evidence-based. In fact, delaying appropriate treatment can increase the risk of:
Permanent nerve injury
Progressive weakness
Reduced mobility
Long-term disability
The Role of Neurosurgery in Chronic Pain Care
Neurosurgery is not about operating on everyone who has pain. In fact, most patients who see a neurosurgeon do not require surgery. The true role of neurosurgery is precision—understanding why pain is occurring, what structures are involved, and when intervention is necessary to prevent long-term harm.
A comprehensive neurosurgical evaluation focuses on answering several critical questions that directly affect your long-term outcome:
Is the pain coming from a structural problem, such as spinal stenosis, disc degeneration, instability, or arthritis, or from irritation or compression of nerves—or both?
Are nerves currently being compressed, and if so, is that compression reversible, or is there a risk of permanent nerve damage if treatment is delayed?
Has conservative care truly addressed the underlying problem, or has it only reduced symptoms temporarily without correcting the cause?
Is continued nonoperative care reasonable, or has the condition reached a point where surgical or advanced procedural treatment is medically appropriate and beneficial?
These determinations are not made based on imaging alone or symptoms alone. They are made by correlating what a patient feels with what we see anatomically and neurologically.
High-quality clinical evidence shows that in appropriately selected patients—particularly those with spinal stenosis, degenerative spine disease, or nerve compression—timely surgical intervention can lead to better long-term pain relief, improved function, and higher quality of life compared with prolonged nonoperative care that fails to address the underlying pathology (New England Journal of Medicine, 2022; The Spine Journal, 2023).
Timing matters. Delaying intervention when nerves are under sustained pressure can allow potentially reversible conditions to become permanent.
Moving Beyond the Myth of “Just Living With It”
One of the most harmful misconceptions patients encounter is the idea that chronic pain should simply be tolerated or accepted as inevitable. While pain is experienced subjectively, its causes are often objectively identifiable through careful clinical evaluation.
Persistent pain is not a character flaw, a weakness, or something that must be endured indefinitely. In many cases, it is a signal that the nervous system or spine is under abnormal stress.
Effective chronic pain care requires:
Careful correlation between symptoms and imaging findings
A detailed neurologic examination, not just a review of scans
Individualized treatment planning, rather than one-size-fits-all protocols
The willingness to intervene when medically indicated, rather than defaulting to indefinite symptom management
Chronic pain should prompt deeper investigation, thoughtful discussion, and informed decision-making—not resignation or dismissal.
The goal is not simply to temporarily reduce pain, but to restore function, protect neurologic health, and improve long-term quality of life.
Why Patients Choose Level One Neurosurgery
At Level One Neurosurgery, chronic pain care is built on evidence, precision, and accountability. Every evaluation begins with a simple principle: patients deserve clarity, not guesswork.
Our focus is not merely short-term pain reduction. It is the protection of neurologic function, the restoration of mobility, and the preservation of long-term quality of life. That requires careful diagnosis, thoughtful treatment planning, and the discipline to intervene only when it is medically justified.
Led by Peter A. Zahos, MD, FAANS, FACS—recognized as a New Jersey Top Doctor and trained in academic neurosurgery—our practice brings the rigor of tertiary-care medicine into a focused, patient-centered setting. This means patients receive the depth of expertise typically found in large academic centers, without fragmentation, delays, or unnecessary escalation.
What sets Level One Neurosurgery apart is not volume—it is judgment:
Careful correlation of symptoms, imaging, and neurologic findings
Honest assessment of whether surgery is necessary—or avoidable
Clear explanations that patients can understand and trust
Decisions grounded in outcomes, not algorithms
Chronic pain is complex, but it is not something patients should simply endure or be dismissed for questioning. In many cases, its causes are identifiable, and its progression can be altered with the right evaluation at the right time.
Chronic pain deserves answers.
At Level One Neurosurgery, those answers are grounded in experience, science, and respect for the individual behind the diagnosis.
Blog Resources:
Raja, S. N., Carr, D. B., Cohen, M., Finnerup, N. B., Flor, H., Gibson, S., Keefe, F. J., Mogil, J. S., Ringkamp, M., Sluka, K. A., Song, X. J., Stevens, B., Sullivan, M. D., Tutelman, P. R., Ushida, T., & Vader, K. (2020). The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain, 161(9), 1976–1982. https://doi.org/10.1097/j.pain.0000000000001939
Chaban V. V. (2021). Mechanisms and Management of Chronic Pain. International journal of research in nursing, 12(1), 1–2. https://doi.org/10.3844/ijrnsp.2021.1.2
Rahman, S., Kidwai, A., Rakhamimova, E., Elias, M., Caldwell, W., & Bergese, S. D. (2023). Clinical Diagnosis and Treatment of Chronic Pain. Diagnostics (Basel, Switzerland), 13(24), 3689. https://doi.org/10.3390/diagnostics13243689
Silverman, S., Schepman, P., Rice, J. B., Robinson, R. L., White, A. G., Fernan, C., & Beck, C. G. (2021). A harm reduction model to assess the impact of new treatments for pain over standard of care among patients with osteoarthritis. Journal of managed care & specialty pharmacy, 27(12), 1652–1660. https://doi.org/10.18553/jmcp.2021.27.12.1652
New Jersey’s Top Doctors. (2025, October 30). New Jersey Monthly. https://njmonthly.com/find-a-doctor/